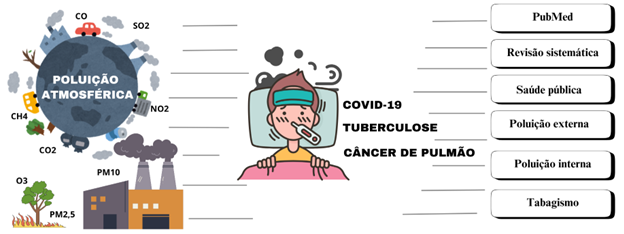
Air pollution as a risk factor for tuberculosis, lung cancer and COVID-19: an integrative literature review
DOI:
https://doi.org/10.58951/dataset.2024.031Keywords:
Air pollution, Pulmonary medicine, Pneumology, Respiratory diseasesAbstract
Since the First Industrial Revolution, air pollution has become an increasingly relevant phenomenon for public health. The adverse effects of various toxic substances or particle clusters, immersed in the air, when in contact with the body are known. These substances and clusters can damage tissues and increase the host's susceptibility to diseases, as well as promote infections by transporting infectious agents. In this sense, the main objective of this review is to analyze the causal or aggravating association between air pollution and the following respiratory diseases: tuberculosis, lung cancer and COVID-19. The studies analyzed indicated that the main parameters linked to tuberculosis are SO2, NO2, CO, O3, PM2.5 and PM10. Although there are uncertainties about the roles of O3. Tobacco, PM2.5, PM10, NO2, O3, SO2, CO, pesticides, crystalline silica and radioactive particles in lung cancer. Even with uncertainties also about the effects of O3. And NO2, SO2, O3, PM2.5 and PM10 to COVID-19. Although there are variations regarding the effects of SO2, the results showed that the parameters interact differently with the respiratory tract and increase its susceptibility to infections, in addition to increasing resistance to cellular replication. Thus, regulation of the amount of these substances in the atmosphere by government authorities can reduce harmful effects on the body and improve public health.
References
Alessio, H. M., Bassett, D. R., Bopp, M. J., Parr, B. B., Patch, G. S., Rankin, J. W., Rojas-Rueda, D., Roti, M. W., & Wojcik, J. R. (2021). Climate Change, Air Pollution, and Physical Inactivity: Is Active Transportation Part of the Solution? Medicine & Science in Sports & Exercise, 53(6), 1170–1178. https://doi.org/10.1249/MSS.0000000000002569 DOI: https://doi.org/10.1249/MSS.0000000000002569
Balmes, J. R. (2019). Household air pollution from domestic combustion of solid fuels and health. Journal of Allergy and Clinical Immunology, 143(6), 1979–1987. https://doi.org/10.1016/j.jaci.2019.04.016 DOI: https://doi.org/10.1016/j.jaci.2019.04.016
Brasil. Instituto Nacional De Pesquisas Espaciais. Programa Queimadas. Brasília: INPE, 2024. Acesso em: 20 set. 2024. Disponível em: https://terrabrasilis.dpi.inpe.br/queimadas/situacao-atual/situacao_atual/.
Brasil. Ministério da Saúde. COVID-19 No Brasil. Brasília: MS, 2024. Disponível em: https://infoms.saude.gov.br/extensions/covid-19_html/covid-19_html.html. Acesso em: 20 set. 2024.
Cobelo, I., Castelhano, F. J., Borge, R., Roig, H. L., Adams, M., Amini, H., Koutrakis, P., & Réquia, W. J. (2023). The impact of wildfires on air pollution and health across land use categories in Brazil over a 16-year period. Environmental Research, 224, 115522. https://doi.org/10.1016/j.envres.2023.115522 DOI: https://doi.org/10.1016/j.envres.2023.115522
Deng, X., Xing, D., Chen, Z., Zou, Y., He, Y., Chen, S., Wang, Q., & Zhang, Y. (2023). The short-term effect of air pollution on the incidence of pulmonary tuberculosis in Chongqing, China, 2014-2020. The Journal of Infection in Developing Countries, 17(12), 1722–1731. https://doi.org/10.3855/jidc.17217 DOI: https://doi.org/10.3855/jidc.17217
Fundação do Câncer. (2024). Câncer de Pulmão No Brasil: por dentro dos números. Rio de Janeroi. Acesso em: 20 set. 2024. Disponível em: <https://www.cancer.org.br/a-fundacao/publicacoes/info-oncollect/>.
Gioda, A., Tonietto, G. B., & Leon, A. P. de. (2019). Exposição ao uso da lenha para cocção no Brasil e sua relação com os agravos à saúde da população. Ciência & Saúde Coletiva, 24(8), 3079–3088. https://doi.org/10.1590/1413-81232018248.23492017 DOI: https://doi.org/10.1590/1413-81232018248.23492017
Grobusch, L. C., & Grobusch, M. P. (2022). A hot topic at the environment–health nexus: investigating the impact of climate change on infectious diseases. International Journal of Infectious Diseases, 116, 7–9. https://doi.org/10.1016/j.ijid.2021.12.350 DOI: https://doi.org/10.1016/j.ijid.2021.12.350
He, Y., Liu, W. J., Jia, N., Richardson, S., & Huang, C. (2023). Viral respiratory infections in a rapidly changing climate: the need to prepare for the next pandemic. EBioMedicine, 93, 104593. https://doi.org/10.1016/j.ebiom.2023.104593 DOI: https://doi.org/10.1016/j.ebiom.2023.104593
Kangkhetkron, T., & Juntarawijit, C. (2021). Pesticide exposure and lung cancer risk: A case-control study in Nakhon Sawan, Thailand. F1000Research, 9, 492. https://doi.org/10.12688/f1000research.24114.4 DOI: https://doi.org/10.12688/f1000research.24114.5
Li, Y., Sun, J., Lei, R., Zheng, J., Tian, X., Xue, B., & Luo, B. (2023). The Interactive Effects between Drought and Air Pollutants on Children’s Upper Respiratory Tract Infection: A Time-Series Analysis in Gansu, China. International Journal of Environmental Research and Public Health, 20(3), 1959. https://doi.org/10.3390/ijerph20031959 DOI: https://doi.org/10.3390/ijerph20031959
Li, Z., Mao, X., Liu, Q., Song, H., Ji, Y., Xu, D., Qiu, B., Tian, D., & Wang, J. (2019). Long-term effect of exposure to ambient air pollution on the risk of active tuberculosis. International Journal of Infectious Diseases, 87, 177–184. https://doi.org/10.1016/j.ijid.2019.07.027 DOI: https://doi.org/10.1016/j.ijid.2019.07.027
Lima, A. K. S. de, Ribeiro, A. A. S., Santos, M. E. de J., Santos, R. de C. R. dos, & Souza, M. P. S. (2023). Alterações cardiorrespiratórias decorrentes da exposição à sílica em mineradores: uma revisão integrativa. Dataset Reports, 2(1). https://doi.org/10.58951/dataset.2023.58 DOI: https://doi.org/10.58951/dataset.2023.58
Liu, C. S., Wei, Y., Danesh Yazdi, M., Qiu, X., Castro, E., Zhu, Q., Li, L., Koutrakis, P., Ekenga, C. C., Shi, L., & Schwartz, J. D. (2023). Long-term association of air pollution and incidence of lung cancer among older Americans: A national study in the Medicare cohort. Environment International, 181, 108266. https://doi.org/10.1016/j.envint.2023.108266 DOI: https://doi.org/10.1016/j.envint.2023.108266
Liu, Q., Xu, S., & Lu, X. (2021). Association between air pollution and COVID-19 infection: evidence from data at national and municipal levels. Environmental Science and Pollution Research, 28(28), 37231–37243. https://doi.org/10.1007/s11356-021-13319-5 DOI: https://doi.org/10.1007/s11356-021-13319-5
Michaud, A., & Leigh, R. (2024). Letter from Canada: Global warming and wildfire smoke pollution emerging as major threats to respiratory health. Respirology, 29(5), 430–431. https://doi.org/10.1111/resp.14716 DOI: https://doi.org/10.1111/resp.14716
OMS - Organização Mundial da Saúde. (2023). Relatório Global Sobre Tuberculose. Geneva: OMS, 2023. Acesso em: 20 set. 2024. Disponível em: <https://www.who.int/teams/global-tuberculosis-programme/tb-reports>.
OMS - Organização Mundial da Saúde. (2022). Tabaco: Envenenando Nosso Planeta. Geneva: OMS, 2022. Acesso em: 20 set. 2024. Disponível em: <https://www.who.int/publications/i/item/9789240051287>.
Pacheco, S. E., Guidos-Fogelbach, G., Annesi-Maesano, I., Pawankar, R., D’Amato, G., Latour-Staffeld, P., Urrutia-Pereira, M., Kesic, M. J., & Hernandez, M. L. (2021). Climate change and global issues in allergy and immunology. Journal of Allergy and Clinical Immunology, 148(6), 1366–1377. https://doi.org/10.1016/j.jaci.2021.10.011 DOI: https://doi.org/10.1016/j.jaci.2021.10.011
Peng, W., Li, H., Peng, L., & Wang, Y. (2022). Effects of particulate matter on hospital admissions for respiratory diseases: an ecological study based on 12.5 years of time series data in Shanghai. Environmental Health, 21(12), 1-12. https://doi.org/10.1186/s12940-021-00828-6 DOI: https://doi.org/10.1186/s12940-021-00828-6
Petersen, A. B., Muffley, N., Somsamouth, K., & Singh, P. N. (2019). Smoked Tobacco, Air Pollution, and Tuberculosis in Lao PDR: Findings from a National Sample. International Journal of Environmental Research and Public Health, 16(17), 3059. https://doi.org/10.3390/ijerph16173059 DOI: https://doi.org/10.3390/ijerph16173059
Plataforma - MapBiomas Brasil (2024). Histórico do fogo no Brasil (1985 a 2023). MapBiomas Fogo Coleção 3. Acesso em: 23 outubro de 2024. Disponível em: https://plataforma.brasil.mapbiomas.org/hotside-fogo.
Puzzolo, E., Fleeman, N., Lorenzetti, F., Rubinstein, F., Li, Y., Xing, R., Shen, G., Nix, E., Maden, M., Bresnahan, R., Duarte, R., Abebe, L., Lewis, J., Williams, K. N., Adahir-Rohani, H., & Pope, D. (2024). Estimated health effects from domestic use of gaseous fuels for cooking and heating in high-income, middle-income, and low-income countries: a systematic review and meta-analyses. The Lancet Respiratory Medicine, 12(4), 281–293. https://doi.org/10.1016/S2213-2600(23)00427-7 DOI: https://doi.org/10.1016/S2213-2600(23)00427-7
Rahimimoghadam, S., Ganjali, A., Khanjani, N., Normohammadi, M., & Yari, S. (2023). Application of Multiple Occupational Health Risk Assessment Models for Crystalline Silica Dust among Stone Carvers. Asian Pacific Journal of Cancer Prevention, 24(11), 3999–4005. https://doi.org/10.31557/APJCP.2023.24.11.3999 DOI: https://doi.org/10.31557/APJCP.2023.24.11.3999
Requia, W. J., Vicedo-Cabrera, A. M., Amini, H., & Schwartz, J. D. (2024). Short-term air pollution exposure and mortality in Brazil: Investigating the susceptible population groups. Environmental Pollution, 340, 122797. https://doi.org/10.1016/j.envpol.2023.122797 DOI: https://doi.org/10.1016/j.envpol.2023.122797
Santibáñez-Andrade, M., Chirino, Y. I., González-Ramírez, I., Sánchez-Pérez, Y., & García-Cuellar, C. M. (2019). Deciphering the Code between Air Pollution and Disease: The Effect of Particulate Matter on Cancer Hallmarks. International Journal of Molecular Sciences, 21(1), 136. https://doi.org/10.3390/ijms21010136 DOI: https://doi.org/10.3390/ijms21010136
Semczuk-Kaczmarek, K., Rys-Czaporowska, A., Sierdzinski, J., Kaczmarek, L. D., Szymanski, F. M., & Platek, A. E. (2022). Association between air pollution and COVID-19 mortality and morbidity. Internal and Emergency Medicine, 17(2), 467–473. https://doi.org/10.1007/s11739-021-02834-5 DOI: https://doi.org/10.1007/s11739-021-02834-5
Tao, B., Li, Z., Wang, Y., Wu, J., Shi, X., Shi, J., Liu, Q., & Wang, J. (2023). Environment pollutants exposure affects the endogenous activation of within-host Mycobacterium tuberculosis. Environmental Research, 227, 115695. https://doi.org/10.1016/j.envres.2023.115695 DOI: https://doi.org/10.1016/j.envres.2023.115695
Urrutia-Pereira, M., Guidos-Fogelbach, G., & Solé, D. (2022). Climate changes, air pollution and allergic diseases in childhood and adolescence. Jornal de Pediatria, 98, S47–S54. https://doi.org/10.1016/j.jped.2021.10.005 DOI: https://doi.org/10.1016/j.jped.2021.10.005
Van Vliet, E. D. S., Kinney, P. L., Owusu-Agyei, S., Schluger, N. W., Ae-Ngibise, K. A., Whyatt, R. M., Jack, D. W., Agyei, O., Chillrud, S. N., Boamah, E. A., Mujtaba, M., & Asante, K. P. (2019). Current respiratory symptoms and risk factors in pregnant women cooking with biomass fuels in rural Ghana. Environment International, 124, 533–540. https://doi.org/10.1016/j.envint.2019.01.046 DOI: https://doi.org/10.1016/j.envint.2019.01.046
Veith, M., McAlarney, D., Xue, X., Rohan, T. E., & Hosgood, H. D. (2021). Characterizing Trends in Lung Cancer Mortality Attributable to Airborne Environmental Carcinogens. International Journal of Environmental Research and Public Health, 18(24), 13162. https://doi.org/10.3390/ijerph182413162 DOI: https://doi.org/10.3390/ijerph182413162
Vergadi, E., Rouva, G., Angeli, M., & Galanakis, E. (2022). Infectious Diseases Associated with Desert Dust Outbreaks: A Systematic Review. International Journal of Environmental Research and Public Health, 19(11), 6907. https://doi.org/10.3390/ijerph19116907 DOI: https://doi.org/10.3390/ijerph19116907
Xing, D. F., Xu, C. D., Liao, X. Y., Xing, T. Y., Cheng, S. P., Hu, M. G., & Wang, J. X. (2019). Spatial association between outdoor air pollution and lung cancer incidence in China. BMC Public Health, 19(1), 1377. https://doi.org/10.1186/s12889-019-7740-y DOI: https://doi.org/10.1186/s12889-019-7740-y
Xu, L., Taylor, J. E., & Kaiser, J. (2022). Short-term air pollution exposure and COVID-19 infection in the United States. Environmental Pollution, 292, 118369. https://doi.org/10.1016/j.envpol.2021.118369 DOI: https://doi.org/10.1016/j.envpol.2021.118369
Yam, E. L. Y. (2020). Climate change and the origin of SARS-CoV-2. Journal of Travel Medicine, 27(8). https://doi.org/10.1093/jtm/taaa224 DOI: https://doi.org/10.1093/jtm/taaa224
Yang, J., Zhang, M., Chen, Y., Ma, L., Yadikaer, R., Lu, Y., Lou, P., Pu, Y., Xiang, R., & Rui, B. (2020). A study on the relationship between air pollution and pulmonary tuberculosis based on the general additive model in Wulumuqi, China. International Journal of Infectious Diseases, 96, 42–47. https://doi.org/10.1016/j.ijid.2020.03.032 DOI: https://doi.org/10.1016/j.ijid.2020.03.032
Zhang, C., Zhao, D., Liu, F., Yang, J., Ban, J., Du, P., Lu, K., Ma, R., Liu, Y., Sun, Q., Chen, S., & Li, T. (2024). Dust particulate matter increases pulmonary embolism onset: A nationwide time-stratified case-crossover study in China. Environment International, 186, 108586. https://doi.org/10.1016/j.envint.2024.108586 DOI: https://doi.org/10.1016/j.envint.2024.108586
Zhang, X., Tang, M., Guo, F., Wei, F., Yu, Z., Gao, K., Jin, M., Wang, J., & Chen, K. (2021). Associations between air pollution and COVID-19 epidemic during quarantine period in China. Environmental Pollution, 268, 115897. https://doi.org/10.1016/j.envpol.2020.115897 DOI: https://doi.org/10.1016/j.envpol.2020.115897
Zhu, F., Yu, H., Fan, X., Ding, Z., Wang, Q., & Zhou, J. (2023). Particulate air pollution and cardiovascular disease mortality in Jiangsu Province, China: a time-series analysis between 2015 and 2021. Frontiers in Public Health, 11. https://doi.org/10.3389/fpubh.2023.1218479 DOI: https://doi.org/10.3389/fpubh.2023.1218479
Zhu, Y., Xie, J., Huang, F., & Cao, L. (2020). Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Science of The Total Environment, 727, 138704. https://doi.org/10.1016/j.scitotenv.2020.138704 DOI: https://doi.org/10.1016/j.scitotenv.2020.138704
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Yuri José Almeida dos Santos, Lilibeth Batista de Maras, Talita Pereira Lima

This work is licensed under a Creative Commons Attribution 4.0 International License.
This journal publishes its Open Access articles under a Creative Commons license (CC BY 4.0).
You are free to:
Share — copy and redistribute the material in any medium or format for any purpose, even commercially.
Adapt — remix, transform, and build upon the material for any purpose, even commercially.
The licensor cannot revoke these freedoms as long as you follow the license terms.
Under the following terms:
Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
Notices:
You do not have to comply with the license for elements of the material in the public domain or where your use is permitted by an applicable exception or limitation.
No warranties are given. The license may not give you all of the permissions necessary for your intended use. For example, other rights such as publicity, privacy, or moral rights may limit how you use the material.




